Watery Eyes / Lacrymal Duct Obstructions
Normally, the excess of continuously producing tear film, after crossing the eye surface, enters into lacrymal drainage system through upper and lower punctum (tiny openings on the inner third of eyelid margins) and travel through the canaliculi to the lacrimal sac and then drain into the nasal cavity via the nasolacrimal duct.As the used tears move away from the eye through the tear ducts, fresh tears come in from glands.
Contraction of the orbicularis muscles (eyelid blinking) creates an 'active pumping' action that facilitates the flow of tears through the lacrimal drainage system.
The obstruction of the lacrimal drainage system present with tearing (epiphora, watering of eye), a complaint frustrating to patients needing always a wiper on hand. Watering may result from obstruction at any level of the lacrimal drainage system which consists a 35 to 37 mm tubular network beginning at the puncta and terminating in the inferior nasal meatus. 
Nasolacrymal duct (NLD) obstruction is the most common clinical entity of lacrymal drainage system causing outflow of tears, epiphora (watery eye). Spontaneous stenosis is probably the most common cause of NLD obstruction in middle age to older persons. It affects women twice as frequently as men. Although the exact inciting event is unknown, anatomical factors in women, allergy and chronic inflammation of nose and paranasal sinuses may play role. A hard cast formation within the lacrimal sac (dacryolith) can also produce obstruction of duct.
Naso-orbital fractures involving the bony structures of NLD (trauma) can cause permenant obstruction.
If there is a mass lesion with an atypical clinical presentation further workup (imaging) would be appropriate to exclude any tumor. Bloody discharge and/or mass lesion is highly suggestive of neoplasm.
Chronic and excessive tearing (watering) is the primary complaint of patients with NLD obstruction, followed by acute or chronic infections leading to sticky mucous, or mucopurulent discharge. Chronic dacryocystitis is an infection or inflammation of the nasolacrimal sac, caused by blockage of the nasolacrimal duct (NLD). Severe pain with local swelling and redness at site close to nose suggests an exacerbation called as "acute dacryocystitis".
Diagnosing dacryocystitis is relatively easy with a history of chronic epiphora and sticky discharge dating back several months or years.
On external examination, visible signs of swelling and redness of lacrimal sac region can be seen. The purulent secretion will come out if pressed on lacrimal sac region.
The definitive diagnosis is usually done by saline injection (lavage) through the canaliculi. The saline will not pass into the nose and come back (together with mucopurulent secretion collected in sac) through the canaliculi.
In some cases, a dye disappearance test may be required. During this test, a drop of the yellow fluorescein dye is instilled into the conjunctival sac. In a healthy eye, the instilled yellow dye will disappear from eye in a few minutes. In case of obstruction, the dye will not drain into nose and not disappear from the eye in a short period of time. The dye disappearance test is especially indicated in partial obstructions or in non-obstructive waterings. The passage of dye into nasal cavity may be checked by a cotton swab. 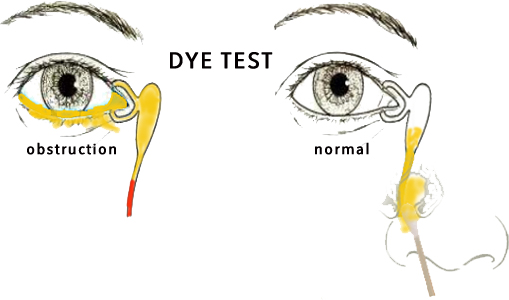
Although topical antibiotic therapy is frequently prescribed for dacryocystitis for the treatment of secondary infection, the definitive treatment of dacryocystitis is surgical.
A dacryocystorhinostomy (DCR) operation, which involves surgical fistulization of the lacrimal sac into the nasal cavity, is done using a variety of techniques. The operative approach to the sac may be external (by skin incision) or endoscopic (through the nose).
Despite gradually ease and decreased morbidity of endonasal DCR, external DCR is still the procedure of choice (gold standard) as it is more successful. Contrary to common asserts, the visible scar at the incision site is extremely rare.
Endonasal approach may be convenient in recurrent cases for revising of soft tissues with an existing bony ostium from previous surgery.
Monocanalicular or bicanalicular silicone tube stents may be placed, if needed, during external DCR surgery, however it is compulsory in all cases during endonasal DCR surgery.
DCR Surgery, although it can be done under local anesthesia with sedation, is usually performed under general anesthesia, which is more comfortable both for the patient and surgeon.
Any obstructions of the lacrimal drainage system other than nasolacrimal duct can be caused by trauma, chronic infections and some cicatricial diseases. These obstructions may require specific and delicate microsurgical techniques with the intubation of specific type of mono or bicanalicular stents or Jones tubes etc.







